Sports Medicine Education No. IV - Patellofemoral Joint Syndrome
Description
Patellofemoral joint (PFJ) symdrome afflicts women twice as often as it does men in adolescents and young adults. However, it occurs about equally among male and felmale athletes. Sports requiring continuous and heavy leg impact, such as track, gymnastic, badminton, aerobics and dancing report a higher incidence of PFJ syndrome than low impact sports. The commonly seen causes include overuse, trauma and malalignment. PFJ syndrome describes the pathology related to the changes of the undersurface of articular cartilage of the patella. It can range from mild irritation and inflammation to macroscopically visible changes at arthroscopy. The most frequently reported symptom is dull aching pain at the front of the knee directly behind the patella which is exacerbated by prolonged sitting, descending hills or stairs, deep knee bends and repetitive flexion / extension exercises. There might also be crepitus, pseudolocking and / or giving way.
Functional anatomy
Diagram 1: The patella normally sits symmetrically in the femoral groove
During flexion, the patella moves in the groove formed by the femoral condyles and comes to lie within the intercondylar notch. If there is soft tissue tightness, muscle weakness, poor muscle control or certain anatomical variations such as knock knees and flat feet, patella maltracking might occur i.e. the patella cannot move smoothly in the groove.
Diagram 2: Compressive forces of the patellofemoral joint
During physical activities that require repetitive knee flexion, patellofemoral compressive force (PFCF) increases as knee flexion increases. For example, PFCF during level walking is 0.5 times body weight; going upstairs is 3-4 times body weight; squatting is 7-8 times body weight.
PFCF is further increased by the factors mentioned above such as muscle tightness and certain anatomical variations.
Treatment
Treatments for PFJ syndrome remain varied and controversial. They range from surgery, rest, medication and physiotherapy. Very often, physiotherapy and activities modification help and is the first choice of treatment.
Physiotherapy aims at:
- Reducing pain and inflammation
- rest, ice, electrical modalities are used
- Correcting abnormal patellar position
- tapes or special braces are used
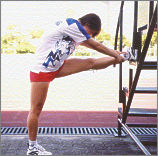
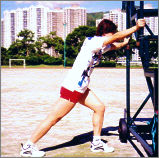
- stretching exercises or mobilization techniques to increase the flexibility of tight structures
 |
 |
 |
 |
- Correcting abnormal biomechanics
- orthotics are prescribed if there is excessive foot pronation
- pelvic control will be taught to stabilize the lateral pelvis and to control external hip rotation
- Strengthening vastus medialis oblique (VMO) and hip adductors
- isometric, fast speed isokinetic and / or closed chain terminal extension exercises (e.g. leg press and squat with limited range) are usually prescribed to minimize PFCF.
- biofeedback device during functional positions can enhance the recruitment of VMO before the rest of the quadriceps.
-
Activities modification
PFCF is minimal when the leg is straight or only slightly bent. The best activities are the ones that limit the knee to a range between 135 degrees (1/4 squat) and 180 degrees (straight) especially when the pain is bad.
These activities will be easiest on the knee:
1. Swimming (flutter kick, knees straight)
2. Cycling (with a high seat)
3. Slow jogging on grass
These activities are hard on the knees and most likely aggravate your condition:
1. bunny hop
2. running (sprints, downhill)
3. climbing stairs (up and down)
Use your judgement. When your knees hurt, avoid all but the good activities. Total rest may be required sometimes. Consult your doctor and / or physiotherapist early so that appropriate management can be implemented.
For more information, please contact:
Sports Medicine Department
Telephone: (852) 2681 6134
All information in this pamphlet is for reference only
 ID: hksportsinstitute
ID: hksportsinstitute

